Study announcement: GALILEO
Transcatheter Aortic Valve Implantation (TAVI)
Cardialysis and Mount Sinai will Conduct New Trans Atlantic Study Launched by Bayer to Evaluate Rivaroxaban in Patients after Successful Transcatheter Aortic Valve Implantation (TAVI)

• Despite the current use of antiplatelet agents, one in every 20-25 patients suffers a stroke or other cardiovascular adverse events within one year following transcatheter aortic valve implantation (TAVI)
• The Phase III GALILEO study will evaluate the potential clinical value of rivaroxaban to improve clinical outcomes by preventing potentially deadly blood clots in patients who have just undergone TAVI
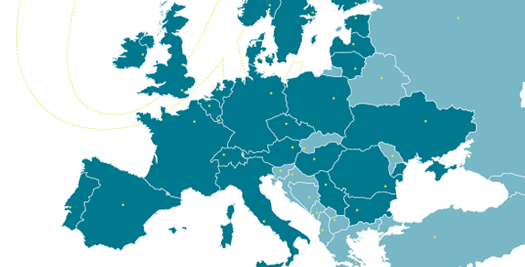
Rotterdam, The Netherlands – 15th May 2015 – Cardialysis and Mount Sinai, in collaboration with Bayer HealthCare and Janssen Research & Development, LLC, announce today the initiation of the GALILEO study to investigate the long-term benefit-risk profile of its oral Factor Xa inhibitor rivaroxaban for the prevention of ischaemic and thromboembolic events – such as stroke, heart attack or pulmonary embolism – in patients after successful transcatheter aortic valve implantation (TAVI). This Phase III study will enroll approximately 1,500 patients in 15 countries worldwide under the scientific leadership of Professors Stephan Windecker and George D. Dangas, from Bern University Hospital, Switzerland, and Icahn School of Medicine at Mount Sinai, New York, USA respectively.
TAVI is a minimally invasive option for patients suffering from aortic stenosis who are inoperable or at increased surgical risk. The prevalence of aortic stenosis is about 5 per cent in people above the age of 75, making it the most common valvular heart disease in the developed world., Significant post-procedural risks for these patients are thrombotic (or blood clot-related) complications and associated mortality, with one in 20-25 patients suffering a stroke or other cardiovascular adverse events within the first year. Current practice is to prescribe post-procedural therapy with dual antiplatelet treatment of acetylsalicylic acid (ASA, indefinitely) plus clopidogrel (for one to six months) based on expert consensus. However, there is no evidence from randomized controlled clinical trials specifically supporting the benefits of antiplatelet therapy after TAVI and the ideal antithrombotic regimen balancing ischaemic and bleeding risk requires further investigation.
“In the GALILEO study we will investigate the clinical benefits of a novel oral anticoagulant-based antithrombotic therapy of rivaroxaban plus ASA for three months followed by rivaroxaban alone thereafter.” said Co-Principal Investigator Prof Stephan Windecker, Chief of Cardiology at Bern University Hospital and President of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). “This study will provide cardiologists with important insights on the optimal antithrombotic treatment after TAVI to prevent thromboembolic events such as stroke, heart attack and a high risk for death.”
“GALILEO aims to answer an important question from the clinical field using the oral Factor Xa inhibitor rivaroxaban to optimize TAVI treatment with a weighed antithrombotic regimen on both sides of the Atlantic Ocean” said Gerrit-Anne van Es, director of Research and Business Development of Cardialysis. “We are very glad that Bayer embraced this clinical study concept, including our academic partnership with Mount Sinai”.
About GALILEO
The Phase III GALILEO study will enroll approximately 1,500 patients after successful TAVI with any approved device, who do not have atrial fibrillation. The primary efficacy endpoint is a composite of all-cause death, stroke, myocardial infarction, valve thrombosis, pulmonary embolism, deep vein thrombosis and systemic embolism. The primary safety endpoint is life-threatening, disabling or major bleeding events. Patients will be randomized to receive either rivaroxaban 10 mg once daily plus ASA 75-100 mg once daily for three months, followed by rivaroxaban 10 mg once daily alone; or clopidogrel 75 mg once daily plus ASA 75-100 mg for three months, followed by ASA 75-100 mg once daily alone.
About Transcatheter Aortic Valve Implantation (TAVI)
Patients with severe aortic stenosis (AS) experience narrowing of the aortic valve, which is progressive and life-threatening. After the onset of symptoms, average survival is 50 per cent at two years and 20 per cent at five years if left untreated. TAVI is a less invasive alternative option compared to surgical aortic valve replacement and currently used for patients who are considered at high risk or even unsuitable for open heart-valve surgery. In Europe and North America, approximately 290,000 elderly patients with severe AS are eligible for TAVI. Nearly 27,000 additional patients become eligible for this procedure every year. TAVI is associated with an increased risk of ischaemic events owing to arterial vessel-wall injury, stent struts exposed to blood flow, and underlying patient risk factors including new onset of atrial fibrillation.
If you would like to learn more about GALILEO please join us at the EuroPCR special symposium entitled “TAVI: current and future perspectives for adjunctive pharmacological therapy.” taking place on Wednesday, 20th May 2015 from 13:35 – 14:35 at Room 251
About Cardialysis
Cardialysis is a leading specialist clinical research organization (CRO) with an exclusive focus on cardiology, providing a full range of clinical research and cardiac Core Laboratory services. Founded in 1983, Cardialysis is recognized for its opinion-leader expertise, strong academic network and in-depth cardiology expertise and in recent years has significantly expanded its operational activities. The world’s top medical device, biotechnology and pharmaceutical companies collaborate with Cardialysis resulting in more than 250 clinical trials conducted up till now, contributing to improved cardiovascular therapies.
Please visit us at our EuroPCR booth (located at N11) or at www.cardialysis.com
Contact Cardialysis:
Gerrit-Anne van Es
Tel. +31 (0)10 - 206 2810
E-Mail: info@cardialysis.nl
About Mount Sinai
The Mount Sinai Health System is an integrated health system committed to providing distinguished care, conducting transformative research, and advancing biomedical education. Structured around seven hospital campuses and a single medical school, the Health System has an extensive ambulatory network and a range of inpatient and outpatient services—from community-based facilities to tertiary and quaternary care.
The System includes approximately 6,600 primary and specialty care physicians, 12-minority-owned free-standing ambulatory surgery centers, over 45 ambulatory practices throughout the five boroughs of New York City, Westchester, and Long Island, as well as 31 affiliated community health centers. Physicians are affiliated with the Icahn School of Medicine at Mount Sinai, which is ranked among the top 20 medical schools both in National Institutes of Health funding and by U.S. News & World Report.
For more information, visit mountsinai.org, or find Mount Sinai on Facebook, Twitter, YouTube and Instagram.
Contact Mount Sinai:
Lauren Woods
Tel. +1 646-634-0869
E-Mail: lauren.woods@mountsinai.org
References
Holmes DR, et al. Clinical outcomes at 1 year following transcatheter aortic valve replacement. JAMA, 2015; 313:1019-1028.
Lindroos M, et al. Epidemiological studies estimate the prevalence of aortic stenosis at 5% in subjects over the age of 75 years. J Am Coll Cardiol, 1993; 21: 1220-5.
Manning WJ (October 2013). "Asymptomatic aortic stenosis in the elderly: a clinical review". JAMA 310 (14): 1490–7.
Holmes DR, et al. Clinical outcomes at 1 year following transcatheter aortic valve replacement. JAMA, 2015; 313:1019-1028.
Alec V, et al. Guidelines on the management of valvular heart disease, European Heart Journal, 2012; 33 (19) 2451-2496.
Osnabrugge, R.L.J, et al. Aortic stenosis in the elderly: Disease prevalence and number of candidates for transcatheter aortic valve replacement: A meta-analysis and modeling study. J Am Coll Cardiol, 2013; 62(11), 1002–1012.